Sciatica refers to pain and/or paraesthesia (adverse ‘mis-feelings’ ranging from numbness or pins and needles to other sensations such as deep aching or burning sensations) that radiate along the path of the sciatic nerve.
It is a widely misunderstood topic and very often either misdiagnosed or missed as a specific symptom. Sciatica in itself is not a ‘stand-alone diagnosis’ but is a symptom of the involved nerve being irritated/affected by another structure, which, is usually the issue (or diagnosis). Sciatica does not occur without an aggravating factor/mechanism.
The Sciatic nerve is the second-largest nerve in the human body. The nerve exits from the bottom of the spine from the 4th Lumbar (lower back) segment to the 3rd Sacral (the solid bone at the base of the spine) segment on each side.
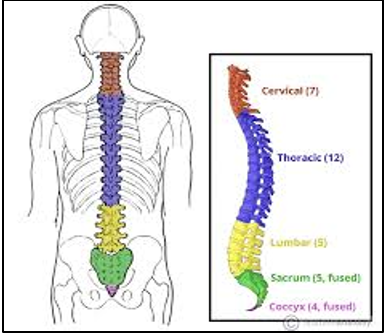

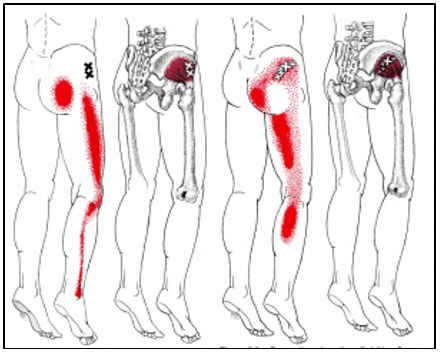
It branches from your lower back through the base of the lower back and buttocks, down the rear of each thigh, and into the rear and outside of the calf plus the soles of the feet. Typically, sciatica affects or presents only on one side of the body but in some more severe cases may present in both lower limbs.


Sciatica most commonly occurs when one (or more) of its exit points from the spine is encroached upon (i.e., it is compressed or irritated by another structure).
Common Causes
May include:
- A bulging disc (protrusion)
- A herniated disc (full prolapse)
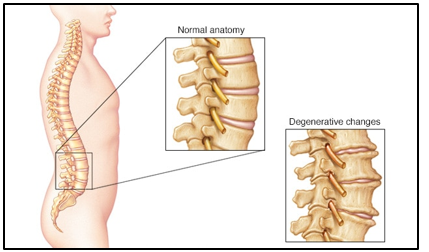
- A spinal bone spur (spondylophyte)
- A narrowing of one or more of the natural nerve exit holes (spinal stenosis) due to general, gradual degeneration processes within the lower spine (spinal stenosis).
- Changes in the mechanical alignment of the lower back/pelvis caused by example by pregnancy or lower limb surgery (such as knee or hip replacement).
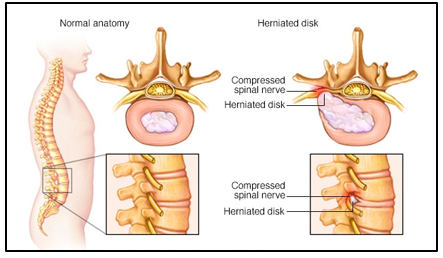
Irritation or compression of a spinal nerve root typically causes it as also other local soft tissue structures to inflame. Inflammation would result in the nerve root and its neighbouring tissue to swell and this, in turn, intensifies the nerve root aggravation resulting in an inflammatory cycle.
Symptoms
Pain that radiates from your lower (lumbar) spine to your buttock and down the back of your leg is the hallmark of sciatica. You might feel the discomfort almost anywhere along the nerve pathway, but it’s especially likely to follow a path from your low back to your buttock and the back of your thigh and calf.
The pain can vary widely, from a mild ache to a sharp, burning sensation that can range intensity from just irritable to excruciating. Sometimes it can feel like a jolt or electric shock.
Some people also have numbness, tingling, or muscle weakness in the affected leg or foot.
You might have pain in one part of your leg and numbness in a completely different part of the leg/foot.
Sciatic symptoms once present can be aggravated by any number of movements, positions, or activities. This is greatly dependent upon the individual’s particular issue causing their ‘Sciatica’. This means that different people with ‘Sciatica’ may well experience different symptom types/symptom levels to each other. Symptoms can also be worse during coughing, sneezing, or even during ‘pressing’ whilst using the toilet.
Risk factors
Risk factors for sciatica include:
- Age– Age-related changes in the spine, such as herniated disks and bone spurs, are the most common causes of sciatica.
- Obesity – By increasing the stress on your spine, excess body weight can contribute to the spinal changes that trigger sciatica.
- Pregnancy
- Occupation– All jobs require repeated monotype positioning and movements. The RSI nature is significantly contributory in regard to lower back conditions, including Sciatica.
- Diabetes – This condition, which affects the way your body uses blood sugar, increases your risk of nerve damage.
Treatment
Although the pain associated with sciatica can be severe, most cases can be resolved with non-operative treatments over a few weeks. People who have severe sciatica that’s associated with significant leg weakness, double leg symptoms, or bowel or bladder changes may be candidates for surgical appraisal.
Mild sciatica can usually be treated with some low-level non-prescription anti-inflammatory medication (seek your local Chemists guidance) and by remaining as mobile/active as possible.
Sciatica does not always respond to painkillers.
If symptoms persist then seeking the input of a health care professional such as a Physiotherapist or Osteopath may be prudent. They will assess the causes of ‘your’ Sciatica and provide various treatment methods to ease/resolve the condition. Frequent treatment methods would include:
- Manual therapy – Hands-on mobilisation of affected tissues/joints/muscles and often the nerve itself). This can be uncomfortable but has a very good track record according to study evidence.
- Acupuncture / Dry needling.
- Exercise therapy – To improve movement, decrease pain, and strengthen the core muscles to support the lower back).
- Education and advice – In effectively managing your daily activities whilst resolving your current condition.
Other treatment pathways may include:
- Prescribed – Higher-strength non-steroidal anti-inflammatory medication (NSAIDs) such as Naproxen, Ibuprofen (antiphlogistic).
- Prescribed – Higher-strength pain killers (analgesics).
- Spinal epidural injection(s) – Direct application of anti-inflammatory and pain-killing substances to the spine/nerve tissue.
- Micro- or partial discectomy – Part removal of the encroaching disc
- Discectomy – Full removal of the involved damaged disc.
- Disc replacement – A relatively new development with mixed evidence outcomes.
- More extensive orthopaedic procedures – Such as spinal fusions or fixations to ‘stabilise’ the involved spinal levels and keep the nerve root free.
- Neural ablation – The destruction (also called ablation) of nerves is a method that may be used to reduce certain kinds of chronic pain by preventing the transmission of pain signals. It is a safe procedure in which a portion of nerve tissue is destroyed or removed to cause an interruption in pain signals and reduce pain responses.
- Neuromodulation – A technology that acts directly upon nerves. It is the alteration—or modulation—of nerve activity by delivering electrical or pharmaceutical agents directly to a target area.
Variances and Differential Diagnosis to ‘Sciatica’
Occasionally other conditions may be taken for ‘classic Sciatica’ (i.e., Sciatica caused by nerve root aggravation). It is not unusual for other body structures to mirror some classic Sciatic symptoms. The following are some examples:
Piriformis Syndrome – Is a condition in which the piriformis muscle, located in the buttock region, spasms and causes buttock pain.
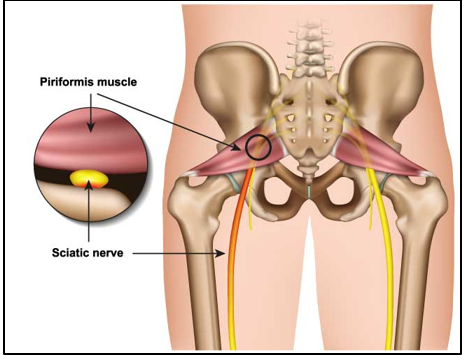
The piriformis muscle can also irritate the nearby sciatic nerve thereby mirroring classic sciatic symptoms within the leg.
Facet Joint Syndrome – ‘Referred pain’ from lower lumbar facet joints can present lower back, buttock, and leg symptoms.

These symptoms can penetrate deep into the thigh, laterally (to the side), and/or posteriorly (to the rear). L4-L5 and L5-S1 facet joints can refer to pain extending into the distal lateral (far outside) leg, and in rarer instances to the foot.
Sacro-Iliac Joint Dysfunctions – Dysfunction in the sacroiliac joint, also called the S.I joint, can sometimes cause lower back and/or leg pain.
Leg pain from sacroiliac joint dysfunction can be particularly difficult to differentiate from radiating leg pain caused by a lumbar disc herniation (sciatica) as they can feel quite similar.
‘Sciatic’ Complications
It is a little-known fact that by adults the spinal cord ends at spinal levels T12 (last thoracic vertebrae) / L1 (first Lumbar Vertebrae). Descending down from this endpoint are nerves that reach down and exit out of the spine at lower levels.
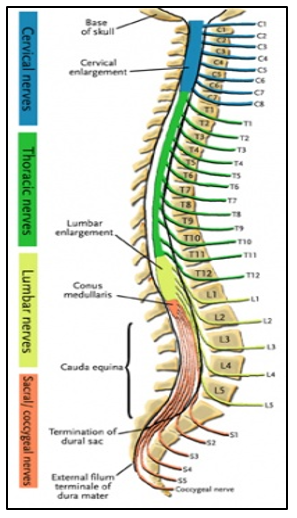
This bunch of nerves is known as the Cauda Equina (translated to English as ‘The horse’s tail’ because its shape resembles this.
The Sciatic nerve is included within the Cauda Equina.
Excessive compression to the spinal cord or Cauda Equina (a large group of nerves, including the Sciatic nerve, located ‘hanging’ below the spinal cord within the spine) can lead to serious problems affecting nerve tissue and its function.
